
Abstract
Noise in hospital environments is a significant yet often marginalized threat to the health of both nurses and midwives and patients. Results from a survey conducted in April 2025 among 65 nurses and midwives in Poland indicate a high level of awareness regarding the negative impact of noise, coupled with a lack of systemic support and implementation of effective acoustic solutions. The situation is particularly critical in neonatal units, which, despite existing standards, often fail to meet basic acoustic requirements.
Introduction
Scientific literature identifies noise as a major environmental stressor in healthcare facilities, affecting not only patients but also medical personnel. Prolonged exposure to high sound levels can lead to sleep disturbances, increased blood pressure, concentration issues, professional burnout, and a higher risk of medical errors.
Particularly vulnerable are preterm and newborn infants, for whom noise can cause neurological developmental disorders, heart rate irregularities, blood pressure issues, and disrupted sleep patterns, according to studies cited by the WHO and international neonatal organizations.
In Poland, the applicable regulation addressing acoustic requirements in healthcare facilities is the PN-B-02151-4:2015-06 standard, which defines acceptable reverberation times and speech intelligibility levels. It has been mandatory for newly constructed or renovated healthcare buildings since 2018. Unfortunately, its enforcement is not systematically controlled, and post-renovation acoustic measurements are not obligatory, leading to significant discrepancies between normative expectations and actual conditions.
Methodology
The survey was conducted on April 4, 2025, during the “Academy of Competence for Nurses and Midwives” conference organized by the Foundation Coalition for the Premature Infant. A total of 65 participants completed the questionnaire, with 64 submitting paper versions. The goal was to gather data on the impact of noise on daily work, the mental and physical health of staff, and patient safety.
Results
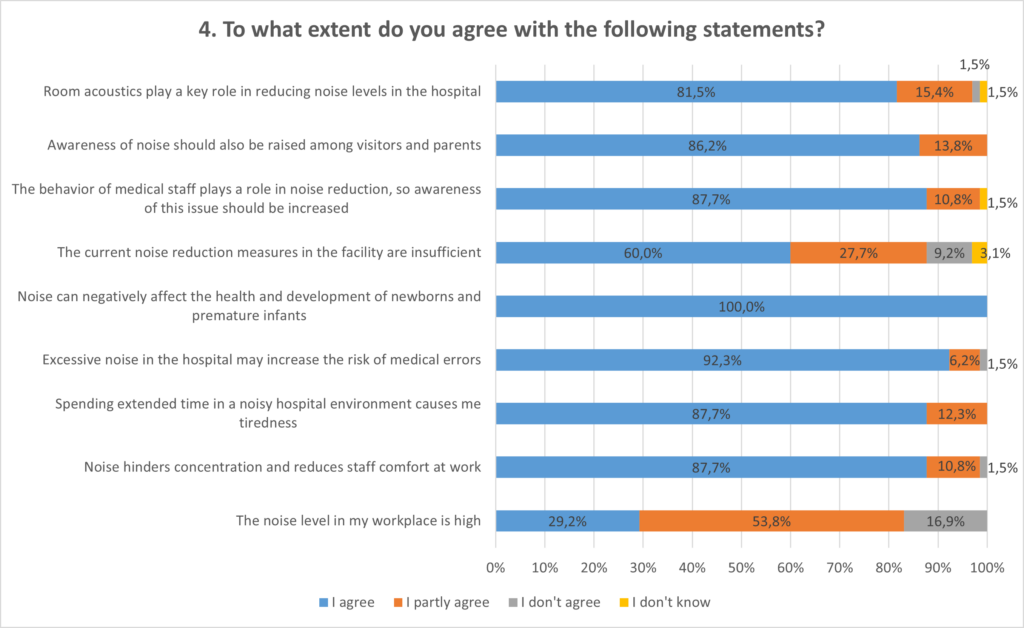
The findings clearly indicate a negative impact of noise:
- 92.3% of respondents believe that noise increases the risk of medical errors.
- 87.7% report increased tiredness and reduced mental comfort.
- 60% consider current actions to be insufficient.
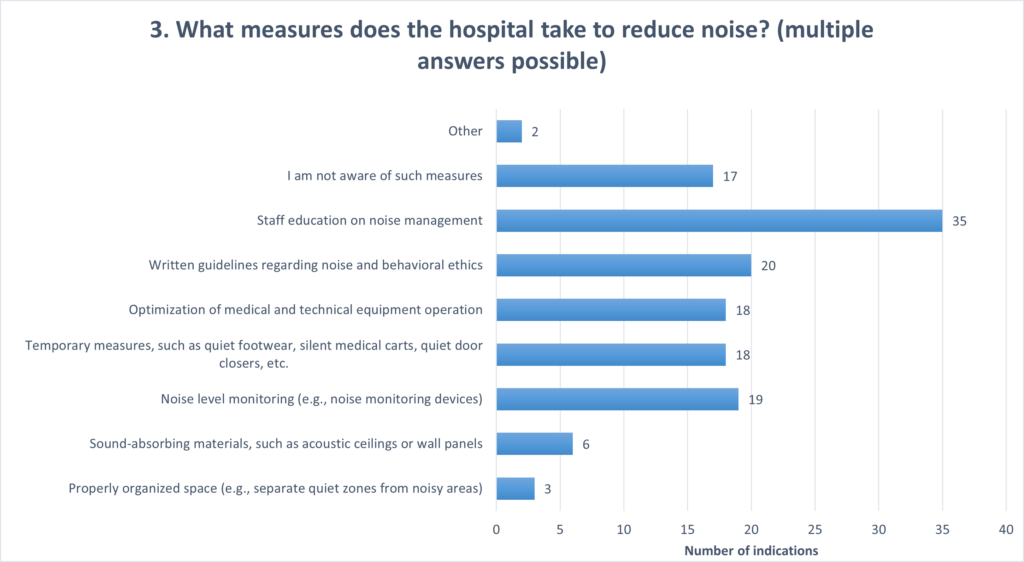
- The most frequently proposed actions include staff education (53.8%) and the implementation of acoustic behavior etiquette (30.8%).
- 100% of respondents confirmed the negative impact of noise on the development of preterm and newborn infants.
Discussion
The results confirm alignment between the subjective perceptions of nurses and midwifes and the findings in scientific literature. Nurses and midwives are aware of the impact of noise, yet they also highlight the lack of tangible actions to improve acoustic quality in their work environments. The prevailing focus on “soft” interventions (education, etiquette), without corresponding infrastructural investment, points to systemic neglect in this area.
It is worth noting that nearly half of the respondents (45%) work in facilities that have not been modernized since 2018, meaning they likely do not meet the requirements of the PN-B-02151-4 standard. The absence of mandatory post-renovation measurements further limits the enforceability of its provisions.
The situation in neonatal units deserves particular attention. Given that all participants identified noise as a threat to preterm infants, and the risks are well documented, implementing mandatory acoustic standards in such units becomes essential. WHO guidelines and design practices demonstrate that effective solutions exist; what is needed now is the will to act.
Conclusions
- Noise is a significant burden on the work of nurses and midwives and a threat to patients, especially newborns.
- The PN-B-02151-4 standard is poorly enforced, and awareness of it remains limited among both healthcare staff and investors.
- Current actions focus mainly on education and etiquette, with a lack of systemic investment in improving acoustic environments.
- Neonatal units should be prioritized when implementing solutions that comply with acoustic standards.
Summary

The survey results constitute a serious wake-up call. Although awareness of the noise issue is high, it is not translating into effective design or management actions. It is time for acoustics to stop being the “invisible problem”. And become a standard component of planning and quality assessment in hospital work environments. Standards, particularly PN-B-02151-4 in Poland, must not only be known but also strictly enforced. Especially in highly sensitive areas such as neonatal care. Where what is at stake is not just comfort but also the safety and development of the most vulnerable patients.
——————————————————————————————————————————————————————————————————————————————————
Please reach out the the author Monika Sadłowska, Concept Developer Healthcare at Saint-Gobain Ecophon Poland, for more detailed information on the research.
Interested in more?
Acoustic comfort assessment in hospital wards: measuring procedures and parameters, by Veronica Amodeo
A holistic assessment of sound environment in hospitals, by Hannah C. W. Jakobsen
Hałas w szpitalach oczami pielęgniarek i położnych – raport z badania 2025 by Monika Sadłowska

